Hey there, health-conscious friend! Let’s talk about something that weighs heavily on many minds: the heart attack. It’s a scary thought, isn’t it? Right up there with cancer and cognitive decline, the fear of a sudden heart event keeps people searching for answers, reassurance, and actionable steps.
- Understanding the Challenge: What Exactly is a Heart Attack?
- Recognizing the Signs: Listening to Your Body’s Signals
- The Power of Proactive Choices: How to Prevent Heart Attack
- Diet: Fueling a Healthy Heart
- Movement: Get Your Body (and Heart) Pumping
- Stress Management: Calming the Cardiovascular System
- Ditch the Smoke: The Single Best Thing for Your Arteries
- Maintain a Healthy Weight: Reducing the Strain
- Exploring Supportive Measures: Supplements for Heart Health
- Key Vitamins and Minerals for Heart Health
- Addressing Concerns: Can Supplements Cause Heart Problems?
- Assessing Your Risk: Understanding Heart Health Tests
- Foundational Tests: EKG and Stress Tests
- Advanced Imaging: Nuclear, Echo, and Calcium Scoring
- The Detailed Look: Coronary CT Angiogram (CCTA)
- Emergency Action: What If You Suspect a Heart Attack?
- Heart Attack vs. Cardiac Arrest: Understanding the Difference
- Frequently Asked Questions (FAQs) on Heart Attack Prevention and Care
- Your Heart Health Journey: Taking Control with Knowledge and Action
You’ve likely wondered, “What are my risks?” or more importantly, “how to prevent heart attack?” That proactive question is exactly where we want to focus today. Because while understanding risks is crucial, prevention is where your true power lies.
I’m here to walk you through it all, like a knowledgeable friend sitting across the table, sharing insights based on science, experience, and a deep understanding of what truly matters for your long-term well-being.
We’ll delve into the early warning signs, including the often-subtle 6 signs of heart attack a month before they might occur (though we need to be realistic about prediction), unpack heart attack symptoms for everyone, paying special attention to heart attack symptoms in women and pre heart attack symptoms female, explore the underlying causes of heart attack, and discuss effective heart attack treatment options.
Crucially, we’ll spend significant time on prevention strategies – the lifestyle choices and supportive measures, including potential heart attack supplements, that can make a world of difference. We’ll even look at the various tests available to assess your risk, cutting through the jargon to understand what they really tell you.
Disclaimer
Before we dive deep, please remember this: I am health enthusiast aiming to provide valuable health information, but this is not medical advice. Always, always consult your trusted physician or cardiologist for personalized diagnosis, treatment, and recommendations regarding your specific health concerns, including discussions about any supplements.
Understanding the Challenge: What Exactly is a Heart Attack?
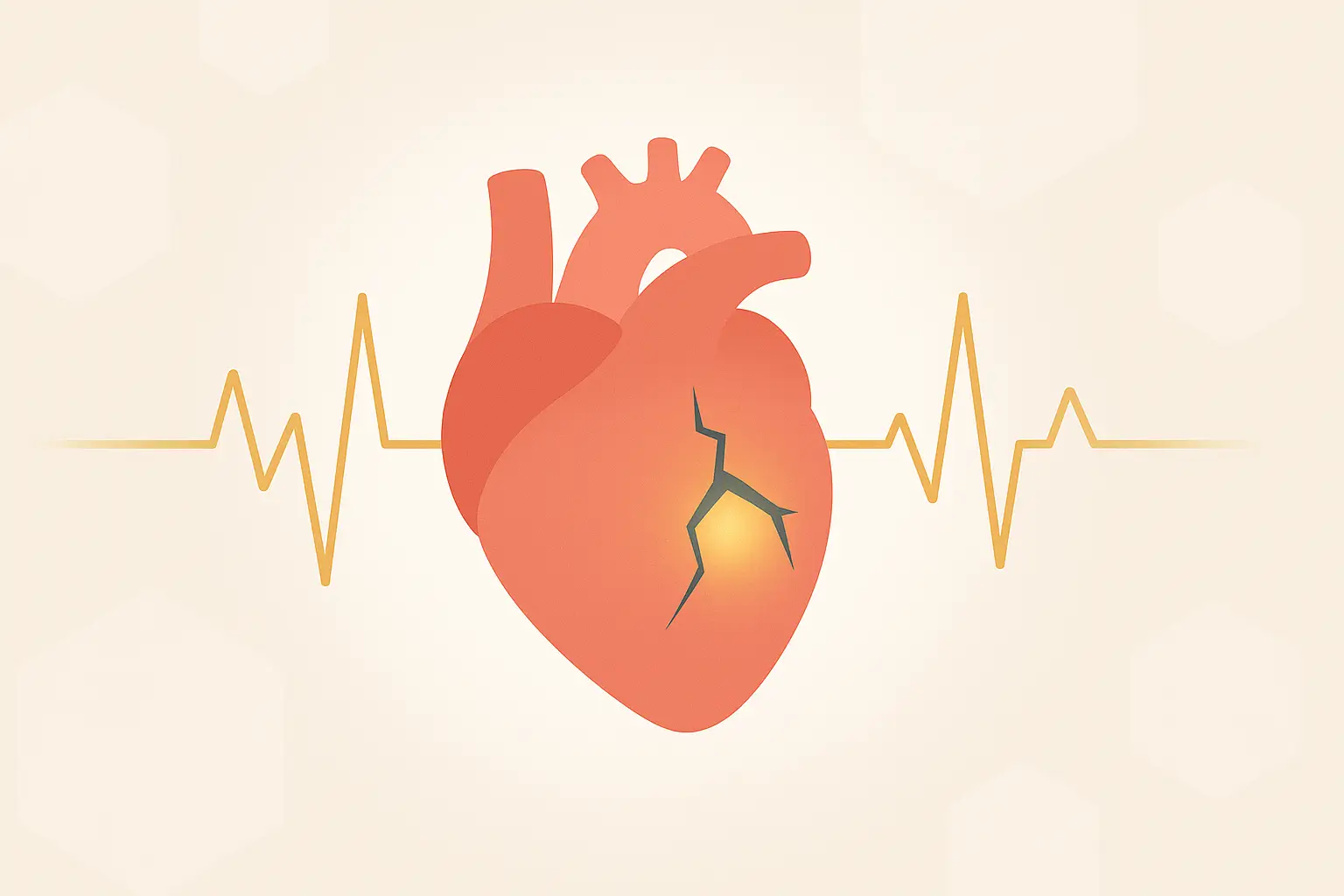
So, what happens during a heart attack, medically known as a myocardial infarction (MI)? In simple terms, it occurs when the blood flow bringing vital oxygen to a part of your heart muscle gets severely reduced or completely cut off. Why does this happen? Most often, it’s due to coronary artery disease (CAD).
Think of your coronary arteries as the fuel lines for your heart muscle. Over time, a combination of fat, cholesterol, calcium, and other substances can build up inside these arteries, forming deposits called plaque. This process is called atherosclerosis. Sometimes, a piece of this plaque can rupture or break open.
When this happens, your body tries to repair the “injury” by forming a blood clot around the ruptured plaque. If that clot grows large enough, it can block the artery, starving the heart muscle downstream of oxygen. Muscle cells deprived of oxygen begin to get damaged and die, leading to a heart attack.
Understanding the causes of heart attack is the first step toward prevention. Key risk factors include:
- High Blood Pressure (Hypertension): Makes your heart work harder and damages artery walls.
- High Cholesterol: Particularly LDL (“bad”) cholesterol contributes to plaque buildup.
- Smoking: Damages blood vessels, reduces oxygen in the blood, and increases blood pressure and heart rate.
- Diabetes: High blood sugar damages blood vessels over time.
- Obesity/Overweight: Often linked to high blood pressure, high cholesterol, and diabetes.
- Lack of Physical Activity: Contributes to obesity, high blood pressure, and high cholesterol.
- Unhealthy Diet: High in saturated/trans fats, sodium, and sugar.
- Stress: Chronic stress can contribute to high blood pressure and other risk factors.
- Age: Risk increases with age.
- Family History: A genetic predisposition can increase risk.
- Sleep Apnea: Can strain the cardiovascular system.
It’s also important to briefly touch upon the different severities or 5 types of heart attacks classifications often used by medical professionals (like the Universal Definition of Myocardial Infarction), which mainly differentiate based on the cause and biomarkers, but for our purposes, understanding the underlying mechanism (blocked blood flow) is key.
Recognizing the Signs: Listening to Your Body’s Signals
Knowing the heart attack symptoms is critical for seeking immediate help. While chest pain is the classic symptom, it’s not always present, and symptoms can vary significantly, especially between men and women.
Common Heart Attack Symptoms:
- Chest Discomfort: Often described as pressure, squeezing, fullness, or pain in the center of the chest. It might last more than a few minutes or go away and come back.
- Pain/Discomfort in Other Upper Body Areas: This can include one or both arms, the back, neck, jaw, or stomach.
- Shortness of Breath: May occur with or without chest discomfort.
- Other Signs: Breaking out in a cold sweat, nausea/vomiting, lightheadedness or dizziness.
Specific Considerations: Heart Attack Symptoms in Women & Pre-Attack Clues
It’s vital to highlight heart attack symptoms in women, as they can be less dramatic and sometimes mistaken for other conditions like the flu, acid reflux, or anxiety. Women are somewhat more likely than men to experience some of the other common symptoms, particularly:
- Shortness of breath
- Nausea/vomiting
- Back or jaw pain
- Unexplained fatigue (lasting days)
- Dizziness or lightheadedness
What about those elusive “6 signs of heart attack a month before”? While there’s no scientifically validated list of six specific signs that reliably predict a heart attack exactly one month out, research does suggest that many people experience pre heart attack symptoms female and male alike in the days, weeks, or even months leading up to a major event.
These can be subtle and intermittent:
- Unusual Fatigue: Profound tiredness not explained by exertion or lack of sleep.
- Sleep Disturbance: Difficulty falling asleep or staying asleep.
- Shortness of Breath: Feeling winded with activities that were previously easy.
- Indigestion or Nausea: Stomach discomfort not related to food.
- Anxiety: A feeling of impending doom or unusual nervousness.
- Mild Chest Discomfort/Pressure: Fleeting or intermittent chest sensations (angina) that might come and go, especially with exertion or stress.
- Pain in Arms, Back, Neck, Jaw, or Stomach: Similar to acute symptoms but potentially milder or intermittent.
The key takeaway: Don’t ignore persistent or unusual symptoms, especially if you have risk factors. Discussing them with your doctor is crucial. These aren’t definitive predictions, but they are signals that something might be amiss and warrants investigation.
The Power of Proactive Choices: How to Prevent Heart Attack
Okay, let’s shift focus to the most empowering part: how to prevent heart attack. While genetics play a role, a huge portion of your heart’s destiny is shaped by your lifestyle choices. This is fantastic news because it means you have significant control!
Diet: Fueling a Healthy Heart
What you eat profoundly impacts heart health. Forget fad diets; focus on sustainable, heart-friendly patterns. The Mediterranean diet is consistently lauded by research for its heart benefits. Key principles include:
- Load Up on Fruits & Vegetables: Aim for a variety of colors. They’re packed with vitamins, minerals, antioxidants, and fiber.
- Choose Whole Grains: Oats, brown rice, quinoa, whole-wheat bread provide fiber that helps manage cholesterol.
- Lean Proteins: Fish (especially fatty fish like salmon rich in Omega-3s), poultry, beans, lentils, and nuts are great choices.
- Healthy Fats: Prioritize unsaturated fats found in olive oil, avocados, nuts, and seeds. Limit saturated fats (fatty meats, full-fat dairy) and strictly avoid trans fats (often found in processed foods).
- Limit Sodium: Excess sodium contributes to high blood pressure. Aim for less than 2,300 mg per day (even less, around 1,500 mg, is ideal for many). Read labels!
- Reduce Added Sugars: Sugary drinks and processed snacks contribute to weight gain, inflammation, and other risk factors. Be mindful of hidden sugars. Consider natural alternatives or high-quality low-calorie sweeteners in moderation, though be aware of ongoing research (some studies, for instance, have investigated potential links like low calorie sweetener heart attack risk, although causality is complex and often debated – moderation and natural choices are usually best).
- Stay Hydrated: Water is essential for overall bodily function, including cardiovascular health.
Building these healthy habits takes consistency. Sometimes, ensuring you get optimal nutrition daily can be challenging with busy lifestyles. While whole foods are paramount, some people find general wellness support helpful. Products focused on hydration and basic nutrient intake, like Forever Aloe Vera Gel®, can complement a healthy diet by supporting digestion and overall well-being, which indirectly benefits heart health management. Always prioritize diet first.
Movement: Get Your Body (and Heart) Pumping
Regular physical activity is non-negotiable for heart health. It helps control weight, lower blood pressure, improve cholesterol levels, and reduce stress. Aim for:
- Aerobic Exercise: At least 150 minutes of moderate-intensity (like brisk walking, cycling, swimming) OR 75 minutes of vigorous-intensity (like jogging, running, interval training) aerobic activity per week.
- Muscle-Strengthening: Include activities targeting major muscle groups (legs, hips, back, abdomen, chest, shoulders, arms) at least two days per week.
- Consistency is Key: Find activities you enjoy! Break it up into smaller chunks if needed (e.g., three 10-minute walks). Start gradually and build up.
Scientific Backing: The American Heart Association (AHA) provides clear guidelines and extensive research supports the link between physical activity and reduced cardiovascular risk. [Insert Link to AHA Physical Activity Recommendations]
Stress Management: Calming the Cardiovascular System
Chronic stress takes a toll on your heart, often leading to high blood pressure, unhealthy behaviors (poor eating, smoking), and direct physiological strain. Finding healthy ways to cope is vital:
- Mindfulness & Meditation: Techniques to focus on the present moment can lower stress hormones. Apps like Calm or Headspace can help.
- Deep Breathing Exercises: Simple, effective, and can be done anywhere.
- Yoga & Tai Chi: Combine physical movement with mindfulness.
- Spending Time in Nature: Proven to reduce stress levels.
- Hobbies & Social Connection: Engaging in enjoyable activities and maintaining strong relationships are powerful stress buffers.
- Adequate Sleep: Aim for 7-9 hours of quality sleep per night. Poor sleep is linked to increased heart risks.
Ditch the Smoke: The Single Best Thing for Your Arteries
If you smoke, quitting is arguably the most impactful step you can take for your heart health. Smoking damages blood vessels, increases plaque buildup, raises blood pressure, and reduces the oxygen your blood can carry. The benefits of quitting start almost immediately. Seek support from your doctor, cessation programs, or resources like Smokefree.gov.
Maintain a Healthy Weight: Reducing the Strain
Carrying excess weight, especially around the abdomen, increases your risk for high blood pressure, high cholesterol, diabetes, and ultimately, heart attack. Even modest weight loss (5-10% of body weight) can significantly improve these markers. Focus on the diet and exercise strategies above for sustainable weight management.
Exploring Supportive Measures: Supplements for Heart Health
While lifestyle is the bedrock of how to prevent heart attack, certain supplements may offer additional support when used appropriately and under medical guidance. It’s crucial to approach this area with caution and knowledge. Supplements are not a replacement for medication or healthy habits.
Let’s explore some key nutrients often discussed in relation to heart health and address common questions and concerns:
Key Vitamins and Minerals for Heart Health
- Omega-3 Fatty Acids (EPA & DHA): Found abundantly in fatty fish. Extensive research suggests Omega-3s can help lower triglycerides, reduce blood pressure slightly, decrease abnormal heart rhythms, and slow the buildup of plaque. They are often considered among the top 5 supplements for heart health. This is particularly relevant for omega 3 supplements after heart attack, often recommended by doctors.

Forever Arctic Sea®
Combines Omega-3s from fish oil with oleic acid from olive oil, providing a source of both EPA and DHA. Discuss with your doctor if this type of supplement fits your needs.
- Magnesium: This mineral plays a crucial role in muscle and nerve function, blood sugar control, and blood pressure regulation. Some studies suggest adequate magnesium intake is linked to lower cardiovascular risk. It’s sometimes explored as one of the best supplements for heart palpitations, although palpitations need medical evaluation first.
- Coenzyme Q10 (CoQ10): An antioxidant your body produces naturally, involved in energy production within cells. Levels may decrease with age or certain conditions. Some research suggests CoQ10 may help improve symptoms of heart failure and potentially lower blood pressure. It’s often included in discussions about the best vitamins for heart and circulation.
- Fiber: Soluble fiber (found in oats, beans, apples) helps lower LDL cholesterol. While best obtained from diet, fiber supplements (like psyllium husk) can help bridge the gap if dietary intake is insufficient.
- Vitamin D: While primarily known for bone health, research is exploring links between Vitamin D deficiency and increased cardiovascular risk factors. Maintaining adequate levels (through sun exposure, diet, or supplements if needed) is important for overall health. Often considered among vitamins for heart health and blood pressure management support.
- Antioxidants (Vitamin C, Vitamin E, Selenium): These help combat oxidative stress, which plays a role in atherosclerosis. While crucial, getting them from a diet rich in fruits and vegetables is generally preferred over high-dose supplements, as research on high-dose antioxidant supplements for heart prevention has yielded mixed results. Some studies even raised concerns about high-dose Vitamin E. This relates to the query about vitamins bad for your heart – excess of certain vitamins can be problematic.
- L-Arginine: An amino acid that helps the body produce nitric oxide, which relaxes blood vessels and improves blood flow. Sometimes discussed for circulation.

Forever ARGI+®
Provides L-Arginine along with a blend of vitamins. As improved circulation is key to heart health, this could be considered supportive, but again, consult a physician, especially if you have existing heart conditions or take medications like nitrates or blood pressure drugs.
This list touches upon some of the best vitamins for heart and brain health too, as good circulation benefits both. For specific needs like womens heart health vitamins, considerations might include ensuring adequate iron (if needed, pre-menopause) and calcium/Vitamin D (post-menopause), alongside the core heart-supportive nutrients.
Looking ahead to the best heart supplements 2025, the focus likely remains on scientifically backed staples like Omega-3s and potentially CoQ10, alongside personalized nutrient strategies based on individual needs and ongoing research.
Addressing Concerns: Can Supplements Cause Heart Problems?
This is a valid and important question. Several keywords reflect this concern: “can supplements cause heart attack or stroke?”, “does supplements cause heart attack?”, “can iron supplements cause heart attack?”, “pre workout supplements heart attack”.
Here’s the breakdown:
- Generally Safe When Used Correctly: Most standard vitamins and minerals, when taken at recommended doses, are safe for most people.
- Potential Risks:
- Interactions: Supplements can interact with prescription medications (e.g., Vitamin K with blood thinners, St. John’s Wort with many drugs). Crucially, inform your doctor about ALL supplements you take.
- Excessive Doses: Taking very high doses of certain supplements can be harmful. We mentioned potential Vitamin E concerns. Does taking calcium supplements increase the risk of heart attack? This is complex. Some large studies suggested a possible link between calcium supplements (especially without adequate Vitamin D or K2) and increased risk, potentially due to calcification of arteries.
However, research is conflicting, and dietary calcium is generally considered safe. It’s a topic to discuss with your doctor, especially regarding dosage and co-supplementation. The same query “do calcium supplements increase risk of heart attack” highlights this ongoing concern. - Stimulants: Pre workout supplements heart attack risk is a real concern. Many contain high doses of caffeine and other stimulants that can dangerously increase heart rate and blood pressure, especially in sensitive individuals or those with underlying conditions.
- Iron: Can iron supplements cause heart attack? Generally, no, unless someone has hemochromatosis (iron overload disorder) or takes excessive amounts unnecessarily. Iron overload can damage organs, including the heart. Only supplement iron if diagnosed with a deficiency.
- Contamination/Quality: The supplement industry isn’t as tightly regulated as pharmaceuticals. Choose reputable brands that undergo third-party testing (like NSF, USP).
- The Bottom Line: Supplements themselves (standard vitamins, minerals, Omega-3s at appropriate doses) are unlikely to directly cause a heart attack in healthy individuals following guidelines. However, interactions, excessive doses, stimulants, underlying conditions, and potentially calcium supplements (in some contexts) require caution and medical consultation.
The focus should always be on supplements to prevent heart attack and stroke as part of a broader healthy lifestyle, not as a magic bullet or potential hazard when used wisely. Post heart attack supplements should only be taken under strict medical supervision.
Assessing Your Risk: Understanding Heart Health Tests
While prevention is key, understanding your individual risk profile can help tailor your efforts. The original article provided a good overview of common tests, often ordered when symptoms arise or risk factors are high. Let’s revisit them with our prevention focus:
(Disclaimer Recap: Remember, your doctor determines which tests, if any, are appropriate for you.)

Foundational Tests: EKG and Stress Tests
- Electrocardiogram (EKG or ECG): A quick, painless snapshot of your heart’s electrical activity. Great for detecting current problems (like an ongoing attack) or signs of past damage. However, as the original article noted, its ability to predict a future heart attack in someone without symptoms is poor. A normal EKG doesn’t mean you’re risk-free.
- Stress Test (Exercise Treadmill Test): Monitors your EKG, heart rate, and blood pressure while you exercise. It helps see how your heart responds to demand and can suggest potential blockages if symptoms or EKG changes occur during exercise. However, its predictive accuracy in asymptomatic people is limited, with both false negatives (missing disease) and false positives (suggesting disease that isn’t there) being possible. It’s relatively inexpensive and safe (risk of major event during test is about 1 in 10,000).
Advanced Imaging: Nuclear, Echo, and Calcium Scoring
When a standard stress test is inconclusive or more detail is needed, doctors might turn to imaging:
- Nuclear Medicine Stress Test (Perfusion Scan): Combines a stress test (exercise or chemical) with injection of a safe radioactive tracer. Images taken before and after stress show how well blood flows to different heart muscle areas.
Better accuracy than a standard stress test (around 88% at identifying significant blockages according to the older meta-analysis mentioned), but still has a notable false-positive rate (around 30% in that analysis, meaning it suggested blockages that weren’t confirmed later). It’s more expensive, time-consuming, and involves a small radiation dose. - Stress Echocardiogram (Stress Echo): Uses ultrasound (echo) to image the heart muscle at rest and immediately after stress (exercise or chemical). Doctors look for changes in how the heart walls move, which can indicate reduced blood flow. No radiation involved. Accuracy is generally comparable to nuclear stress tests.
- Coronary Calcium Score Test (CCST): A specialized CT scan (no dye needed) that measures the amount of calcified plaque in your coronary arteries. Calcium is a marker for atherosclerosis (CAD). The higher the score, the more plaque is present, and generally, the higher the risk of future heart attack. It involves radiation (roughly equivalent to 10 chest X-rays or 1 millisievert). It’s relatively quick but often not covered by insurance (though cash prices can be low, ~$100).
- Accuracy Nuance: As the original piece rightly pointed out, the predictive value depends heavily on the person being tested (“pre-test probability”). A high score in a 75-year-old is less surprising than in a 45-year-old. It’s most informative for middle-aged individuals with intermediate risk factors to help clarify their risk level. It tells you if plaque is present and how much, but not necessarily how narrowed the arteries are.
The Detailed Look: Coronary CT Angiogram (CCTA)
This is often considered the most detailed non-invasive test for evaluating coronary arteries.
- Coronary CT Angiogram (CCTA): Uses advanced CT scanning combined with an intravenous injection of contrast dye. This provides detailed 3D images of the heart and arteries, allowing doctors to see not only if blockages are present but also where they are and how severe the narrowing is.
- High Accuracy: It’s very good at identifying significant blockages (around 95% sensitivity) and quite accurate overall (around 83% specificity, meaning it’s good at ruling out disease when it’s not there). These numbers approach those of the “gold standard” invasive cardiac catheterization.
- Identifying Risky Plaque: Crucially, CCTA can often distinguish between “hard,” calcified plaque (more likely to cause stable angina/chest pain with exertion) and “soft,” non-calcified plaque. These softer plaques are considered more unstable and more likely to rupture, triggering the clot that causes a heart attack or sudden death. Often, the most dangerous plaques only cause moderate narrowing (e.g., 40-70%) before they rupture.
- Downsides: It’s expensive, involves a higher radiation dose than a calcium score (though modern scanners are improving), and requires iodine-based contrast dye, which carries a small risk of allergic reaction or kidney issues in susceptible individuals.
Which Test is “Best”? There’s no single answer. The original article rightly concluded CCTA offers the most comprehensive view non-invasively.
However, the best approach often involves combining information: your symptoms, risk factors (smoking, blood pressure, cholesterol, diabetes, family history), potentially blood tests (like cholesterol panels, maybe Lp(a) – a specific genetic cholesterol marker), and then selecting imaging tests strategically if needed based on that overall picture.
For many people focusing on prevention, diligently managing risk factors is the most powerful test of all!
Emergency Action: What If You Suspect a Heart Attack?
Knowing how to prevent heart attack is goal #1. But recognizing and reacting quickly if symptoms occur is vital.
- Call Emergency Services IMMEDIATELY: Don’t delay. Don’t try to drive yourself. Call 911 (or your local emergency number) right away. Every minute counts; faster treatment means less heart damage. Paramedics can start treatment en route.
- Stop Activity & Rest: Sit or lie down comfortably.
- Chew Aspirin (If Advised): If you are not allergic and don’t have bleeding issues, emergency dispatchers may advise you to chew one regular-strength (325 mg) or 2-4 low-dose (81 mg) aspirin. Aspirin helps thin the blood and can reduce clot formation. Do not take it if you are allergic or told not to.
- Nitroglycerin: If you have been prescribed nitroglycerin for chest pain, take it as directed.
- Stay Calm: As much as possible, try to remain calm while waiting for help.
What about “how to stop a heart attack in 30 seconds?” This phrase is misleading and dangerous. There is no reliable way for an individual to stop a heart attack in progress in 30 seconds at home. The critical action is immediate recognition and calling for professional medical help. Time is muscle!
Emergency Heart Attack Treatment: Once under medical care, heart attack treatment aims to restore blood flow quickly. This may involve:
- Medications: Aspirin, antiplatelets, beta-blockers, ACE inhibitors, statins, nitroglycerin, pain relievers.
- Oxygen Therapy.
- Procedures:
- Angioplasty and Stenting: A thin tube (catheter) with a balloon is threaded to the blocked artery. The balloon is inflated to open the artery, and often a mesh tube (stent) is placed to keep it open.
- Bypass Surgery (CABG): Healthy blood vessels from elsewhere in the body are used to create new routes around the blocked coronary arteries.
Heart Attack vs. Cardiac Arrest: Understanding the Difference
These terms are often confused, but they are not the same. Keywords like “heart attack vs cardiac arrest” and “cardiac arrest vs heart attack” highlight this common point of confusion.
- Heart Attack: A circulation problem. Blood flow to the heart muscle is blocked. The heart is usually still beating (though perhaps erratically or weakly), and the person is typically awake initially.
- Cardiac Arrest: An electrical problem. The heart malfunctions and suddenly stops beating effectively. The person loses consciousness, stops breathing normally (or gasps), and has no pulse. A heart attack can sometimes trigger a cardiac arrest, but they can also happen independently (e.g., due to severe arrhythmias).

Immediate response to Cardiac Arrest: Call 911, start CPR immediately, and use an Automated External Defibrillator (AED) if available.
Frequently Asked Questions (FAQs) on Heart Attack Prevention and Care
Let’s tackle some common questions directly:
Q: What is the most powerful heart supplement?
There’s no single “most powerful” supplement. Effectiveness depends on individual needs and health status. However, Omega-3 fatty acids (EPA/DHA) have arguably the most robust scientific backing for various heart benefits (triglycerides, potential rhythm support).
Always discuss with your doctor before starting any supplement, especially considering it alongside lifestyle changes, which are the most powerful foundation.
Q: What are the 3 tablets for heart attack?
This likely refers to common emergency or initial treatments. While protocols vary, key medications often include:
- Aspirin: To help thin the blood and reduce clotting.
- Nitroglycerin: To relax blood vessels and improve blood flow (often given under the tongue).
- Antiplatelet Medication (like Clopidogrel or Ticagrelor): Often given alongside aspirin to further prevent clot formation.
This is for informational purposes only; medical professionals determine actual treatment.
Q: Which vitamin reduces heart attack?
No single vitamin definitively “reduces” heart attacks on its own as a primary prevention method in large-scale studies.
While adequate levels of vitamins like D and B vitamins are important for overall cardiovascular health, and antioxidants (like C and E) play a role, focusing on a balanced diet rich in various vitamins and minerals from whole foods is more effective than relying on a single vitamin supplement for prevention.
Omega-3s (technically fatty acids, not vitamins) have stronger evidence for specific benefits.
Q: What can I take daily to prevent heart attack?
The most effective daily “prescription” for prevention involves lifestyle choices:
- Eat a heart-healthy diet (fruits, veggies, whole grains, lean protein, healthy fats).
- Engage in regular physical activity.
- Manage stress effectively.
- Avoid smoking.
- Maintain a healthy weight.
- Manage existing conditions (blood pressure, cholesterol, diabetes) with prescribed medications if necessary.
Some people, under doctor’s guidance, might take daily low-dose aspirin (secondary prevention after an event, or primary prevention in specific high-risk cases – never start aspirin daily without consulting a doctor) or specific supplements like Omega-3s if deemed beneficial for their profile.
Q: What is the emergency treatment for a heart attack?
Emergency treatment starts with calling 911. In the hospital, it focuses on rapidly restoring blood flow using medications (aspirin, antiplatelets, blood thinners, etc.) and often procedures like angioplasty with stenting or, less commonly now in the acute phase, bypass surgery. Oxygen and pain management are also key.
Q: How to stop a heart attack in progress?
A: An individual cannot reliably “stop” a heart attack at home. The crucial actions are:
- Recognize symptoms.
- Call 911 immediately.
- Chew aspirin if advised by dispatch/not contraindicated.
- Rest.
Stopping the heart attack process requires professional medical intervention to reopen the blocked artery.
Your Heart Health Journey: Taking Control with Knowledge and Action
We’ve covered a vast amount of ground today, from understanding the mechanics and causes of heart attack to recognizing diverse heart attack symptoms (including pre heart attack symptoms female and the idea of 6 signs of heart attack a month before), exploring diagnostic tests, differentiating heart attack vs cardiac arrest, and outlining heart attack treatment.
Most importantly, we’ve focused heavily on how to prevent heart attack through powerful lifestyle choices – diet, exercise, stress management, smoking cessation, and weight control.
We also navigated the complex world of heart attack supplements, highlighting potential supportive players like Omega-3s (perhaps via options like Forever Arctic Sea®), Magnesium, and CoQ10, while emphasizing the need for caution, medical guidance, and awareness of concerns like can supplements cause heart attack or stroke (generally low risk if used wisely, but interactions and stimulants are key concerns).
We’ve looked at the best vitamins for heart and circulation and addressed specific queries like does taking calcium supplements increase the risk of heart attack.
Your heart health is precious. Empowering yourself with this knowledge is the first step. The next, most crucial step is action. Start small if you need to. Choose one area – maybe adding a daily walk, swapping sugary drinks for water, or incorporating more vegetables into your meals. Build momentum.
Talk to your doctor about your personal risk factors and develop a tailored prevention plan. Discuss any supplements you’re considering, like those targeting vitamins for heart health and blood pressure or the top 5 supplements for heart health, ensuring they fit your specific needs and won’t interact with other medications.
Here at Vitaleap, we’re committed to supporting your journey to vibrant health. Keep exploring, keep learning, and most importantly, keep taking those positive steps for your heart. You’ve got this!