Hey there, health explorer. Let’s talk about something huge in the world of health: hypertension.
- Unpacking Hypertension: More Than Just High Pressure?
- Flow Over Force: What Your Body Really Cares About
- The Kidney Connection & RAAS: A Powerful System That Can Go Rogue
- The Unsung Hero (or Villain?): Endothelial Dysfunction & Stiff Arteries
- Measuring What Matters: Is Pulse Wave Velocity (PWV) the Missing Link?
- Taking the Wheel: Strategies for Healthy Arteries and Blood Pressure
- 1. Move Your Body (The Non-Negotiable!)
- 2. Fuel Wisely: Your Diet Matters Immensely
- 3. Master Your Stress
- 4. Maintain a Healthy Weight
- 5. Ditch the Tobacco
- 6. Consider Supportive Nutrients & Botanicals
- Addressing Specific Concerns About Hypertension
- Reclaiming Your Power in the Hypertension Narrative
You hear the term everywhere, right? Maybe your doctor mentioned it, or you saw a news report.
It often comes with a standard script: monitor your numbers, maybe take a pill, keep it under control.
But what if I told you there might be more to the story?
What if the number on the blood pressure cuff, while important, isn’t the only thing we should be laser-focused on?
Could focusing solely on pressure be like treating a fever without asking why the fever started in the first place?
It’s a big thought, I know. Especially when you consider how common hypertension is.
Statistics suggest a staggering number of us might face this diagnosis, often leading to lifelong medication. The American Heart Association notes that nearly half of adults in the US have high blood pressure.
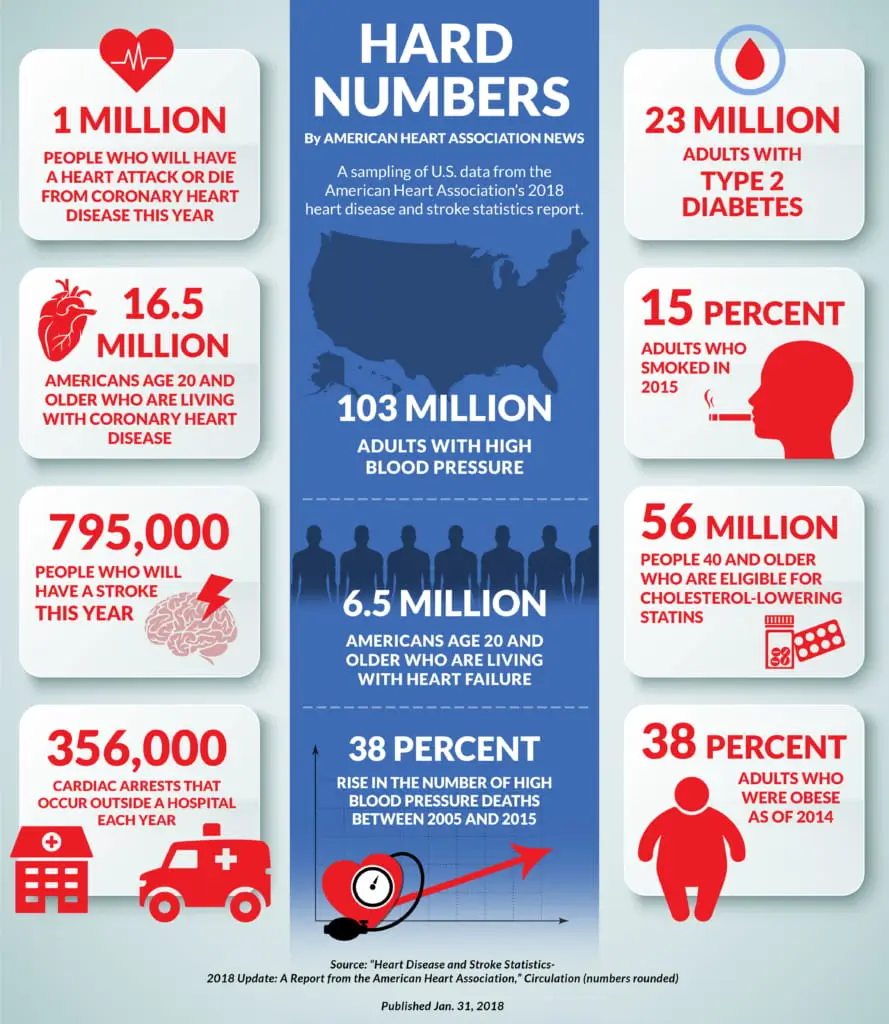
That’s a massive number of people potentially caught in a cycle.
And let’s be honest, the pharmaceutical industry certainly benefits from this widespread diagnosis. We’re talking billions of dollars globally tied to anti-hypertensive medications.
Now, please hear me clearly: high blood pressure is serious. It’s a major risk factor for heart attack, stroke, kidney disease, and more. We absolutely need to take it seriously.
But how we approach it matters.
What if there’s a deeper layer? A way to understand the why behind the pressure?
What if we could look beyond the symptom and towards the underlying health of our arteries?
This isn’t about dismissing current medical advice. It’s about adding a crucial layer of understanding.
It’s about empowering you with knowledge the standard narrative might overlook.
Because true health isn’t just about managing numbers; it’s about understanding and nurturing the incredible system that is your body.
Over the next few minutes, we’ll explore this together. We’ll look at what hypertension really means, beyond just the pressure reading.
We’ll dive into how your body actually regulates things and why focusing on the flow of blood and the health of your arteries might be the key.
And most importantly, we’ll discuss actionable steps – focusing on prevention of hypertension and natural support – that you can take today to potentially influence your long-term cardiovascular health, maybe even before hypertension symptoms ever appear.
So, grab a comfortable seat, maybe a glass of water, and let’s explore this hypertension puzzle together. You might be surprised by what you discover.
Unpacking Hypertension: More Than Just High Pressure?
Let’s start with the basics. What is the hypertension definition or hypertension meaning doctors use?
Technically, hypertension is the medical term for persistently high arterial blood pressure.
Think of your arteries as flexible hoses carrying blood from your heart to the rest of your body. Blood pressure is the force of that blood pushing against the artery walls.
It’s measured in millimeters of mercury (mmHg) and given as two numbers: systolic (the pressure when your heart beats) over diastolic (the pressure when your heart rests between beats).
You’ve likely heard about different stages, like hypertension stage 1 and hypertension stage 2, which indicate increasing levels of pressure and associated risk.
- Stage 1 Hypertension: Systolic between 130-139 mmHg OR diastolic between 80-89 mmHg.
- Stage 2 Hypertension: Systolic 140 mmHg or higher OR diastolic 90 mmHg or higher.
There are also various types of hypertension.
Most common is essential hypertension (or primary hypertension), meaning there’s no single identifiable cause – it likely develops over time due to a combination of genetics, lifestyle, and aging.
Then there’s secondary hypertension, caused by an underlying condition like kidney disease, thyroid problems, or certain medications.
We also see specific types like pulmonary hypertension (high pressure in the arteries of the lungs), portal hypertension (often related to liver disease), gestational hypertension (developing during pregnancy), orthostatic hypertension (blood pressure spikes upon standing), and sometimes severe forms like malignant hypertension. There’s even idiopathic intracranial hypertension (high pressure around the brain).
For classification purposes, medical professionals might use codes like hypertension icd 10 for record-keeping.
So yes, high pressure is the defining feature. But is that the root issue?
The original article made a fascinating point: the word “hypertension” literally means over-stretching. Tension, like in a rubber band, not just pressure.
This hints that the condition of the artery walls themselves – their elasticity or stiffness – might be fundamentally important.
Think about it: A stiff, narrow pipe requires more force to push the same amount of fluid through compared to a flexible, wider one.
Could it be that the high pressure is often a consequence of changes happening within the arteries?
This leads us to a crucial question explored by pioneers like Frederick Akbar Mahomed back in the 1800s: what’s more critical for our body – the pressure itself, or the flow of blood delivering vital oxygen and nutrients?
Let’s dig into that.
What is the cause of hypertension?
Often, for essential hypertension, there isn’t one single cause. It’s usually a mix of genetics, aging, and lifestyle factors like diet, exercise, stress, and weight. Secondary hypertension has specific underlying medical causes. We’ll explore the mechanisms behind rising pressure soon.
What is considered high blood pressure?
Generally, readings consistently above 130/80 mmHg are considered elevated or high, falling into hypertension stage 1 or hypertension stage 2.
Flow Over Force: What Your Body Really Cares About
Imagine your body is a bustling city. Your organs (brain, heart, kidneys, muscles) are the vital districts. Blood vessels are the roads, and blood is the delivery truck fleet carrying essential supplies like oxygen and nutrients.

What’s the absolute top priority for this city to function? Keeping those deliveries moving!
If a critical district like the brain or heart doesn’t get its supplies (blood flow), it’s an immediate crisis.
High traffic (pressure) on the roads is a problem, yes, but a complete standstill (lack of flow) is catastrophic.
Your body instinctively understands this. Mother Nature seems to have prioritized ensuring adequate flow above all else.
Think about basic physics: Pressure = Flow × Resistance.
“Resistance” here refers to how difficult it is for blood to flow through the vessels. Narrower, stiffer vessels mean higher resistance.
Your body is constantly adjusting this resistance to maintain flow.
How? Primarily through the autonomic nervous system, specifically the sympathetic nervous system (your “fight or flight” controller).
This system sends signals to tiny muscles in your blood vessel walls, telling them to constrict (narrow) or relax (widen). More constriction means higher resistance.
Interestingly, research suggests that sometimes, to maintain adequate flow to vital organs, especially if resistance is increasing elsewhere, the body might need to increase pressure [Source: Guyton & Hall Textbook of Medical Physiology – discussion on autoregulation].
It’s a complex balancing act.
Now, here’s a mind-bender from the original article: does your body even have direct pressure sensors in the way we might think?
We often hear about “baroreceptors” located in major arteries like the aorta and carotid arteries (in your neck). The name implies pressure sensing (“baro” means pressure).
But technically, these are stretch receptors. They sense how much the artery wall is stretching with each heartbeat.
More stretch (usually due to higher pressure/volume) signals the brain to dial back the sympathetic nervous system, slowing the heart and relaxing vessels to lower pressure.
Less stretch signals the opposite: ramp up the system to increase pressure and flow.
It’s a rapid response system, crucial for short-term adjustments, like when you stand up suddenly.
But notice the nuance: it’s responding to the stretch of the vessel wall, which is influenced by pressure but also by the stiffness of the wall itself. A stiffer wall stretches differently than a flexible one, even at the same pressure.
This system works around a “set point”—a sort of default pressure/flow range the body aims for. We’ll come back to how this set point can unfortunately get pushed higher over time.
So, while pressure is involved, the body’s immediate regulatory mechanisms seem more directly tuned into flow dynamics and vessel wall stretch/tension.
But there’s another major player in the long-term regulation game, especially involving one organ that’s incredibly sensitive to blood flow: the kidneys.
Can stress cause hypertension?
Yes, absolutely. Chronic stress keeps your sympathetic (“fight or flight”) system activated. This constricts blood vessels, increases heart rate, and can contribute to persistently high blood pressure over time. Managing stress is a key part of prevention of hypertension.
What does high blood pressure mean?
It means the force of blood pushing against your artery walls is consistently too high. This strains your heart and blood vessels, increasing the risk of serious health problems.
The Kidney Connection & RAAS: A Powerful System That Can Go Rogue
Your kidneys are amazing filtration plants. They clean your blood, manage fluid balance, and regulate electrolytes – all crucial jobs that require steady, adequate blood flow.
If blood flow to the kidneys drops, they sound the alarm.
Their main defense and regulation tool is a complex hormonal cascade called the Renin-Angiotensin-Aldosterone System (RAAS).
Understanding RAAS is key to understanding the pathophysiology of hypertension and why many high blood pressure medications work the way they do.
Here’s a simplified breakdown:
- Low Flow Detected: When kidneys sense reduced blood flow (or pressure, or sodium levels drop), they release an enzyme called Renin.
- Angiotensinogen to Angiotensin I: Renin acts on a protein from the liver called Angiotensinogen, converting it into Angiotensin I. This form is mostly inactive.
- ACE Does Its Thing: As blood flows through the lungs (and other tissues), another enzyme called Angiotensin-Converting Enzyme (ACE) converts Angiotensin I into Angiotensin II (ANG II).
- Angiotensin II Takes Action: ANG II is the powerhouse here. It does several things to raise blood pressure:
- Vasoconstriction: It strongly constricts smaller blood vessels (arterioles) throughout the body, increasing resistance and thus pressure. It’s one of the body’s most potent vasoconstrictors.
- Aldosterone Release: It signals the adrenal glands (on top of your kidneys) to release another hormone called Aldosterone.
- Sodium & Water Retention: Aldosterone tells the kidneys to hold onto more sodium and water, increasing blood volume, which also raises pressure.
- Sympathetic Boost: It can also stimulate the sympathetic nervous system, further increasing heart rate and constriction.
Think of RAAS as a survival mechanism designed to ensure vital organs get enough blood flow, especially in situations like dehydration or blood loss.
In a healthy body, this system is beautifully self-regulating with feedback loops [Source: Nature Reviews Nephrology – Overview of RAAS].
However, problems arise when RAAS becomes chronically overactive.
Imagine this system running in overdrive constantly, even when there isn’t a real flow crisis.
The result? Persistent vasoconstriction, increased blood volume, and chronically elevated blood pressure – hello, essential hypertension.
Many common high blood pressure medications target this system:
- ACE Inhibitors: Block the ACE enzyme, reducing the production of Angiotensin II.
- ARBs (Angiotensin II Receptor Blockers): Prevent Angiotensin II from binding to its receptors on blood vessels and other tissues.
- Diuretics (“Water Pills”): Help the kidneys remove excess sodium and water, reducing blood volume.
- Beta-Blockers: Reduce the effects of the sympathetic nervous system on the heart and blood vessels.
- Calcium Channel Blockers: Help relax blood vessel muscles.
These medications can be life-saving and are crucial for managing high blood pressure treatment for many people. They directly address the mechanisms raising the pressure.
But the question remains: Why does RAAS become chronically overactive in the first place for so many people with essential hypertension?
Often, the trail leads back to the health of the blood vessel lining itself.
What are the 10 causes of high blood pressure?
It’s tough to list just 10 definitive causes for essential hypertension, as it’s multifactorial. However, major contributing factors include: unhealthy diet (high sodium, low potassium), lack of physical activity, obesity, chronic stress, smoking, excessive alcohol consumption, older age, genetics/family history, chronic kidney disease, and sleep apnea. Underlying conditions cause secondary hypertension.
What does high blood pressure feel like?
Often, it feels like nothing! That’s why it’s called the “silent killer.” Most people have no high blood pressure symptoms until it causes serious damage.
Occasionally, very high pressure might cause hypertension headache, dizziness, shortness of breath, or nosebleeds, but these aren’t reliable indicators. Relying on feelings is dangerous; regular checks are essential.
The Unsung Hero (or Villain?): Endothelial Dysfunction & Stiff Arteries
Let’s zoom in on the inner lining of your arteries. It’s a super-thin, single layer of cells called the endothelium.
Think of it like a delicate, non-stick coating inside your plumbing.
A healthy endothelium is crucial for cardiovascular health. It does several vital jobs:
- Barrier Function: It controls what passes from the blood into the artery wall (like keeping out “bad” LDL cholesterol).
- Regulates Tone: It produces substances that help vessels relax or constrict. The most famous relaxing substance is Nitric Oxide (NO). NO is a potent vasodilator – it tells the artery muscles to chill out, keeping vessels flexible and open (compliant).
- Prevents Clots: It helps keep blood flowing smoothly.
When this delicate lining gets damaged or isn’t working properly, we call it endothelial dysfunction.
What causes this damage? The usual suspects often implicated in the causes of hypertension:
- High blood sugar (diabetes or pre-diabetes)
- Smoking
- High LDL (“bad”) cholesterol and triglycerides
- Chronic inflammation
- Oxidative stress (an imbalance between damaging free radicals and protective antioxidants)
- High blood pressure itself (it’s a vicious cycle!)
- Lack of physical activity
- Unhealthy diet (high in processed foods, unhealthy fats, sugar; low in fruits, vegetables, fiber)
When the endothelium is dysfunctional:
- NO Production Drops: Less nitric oxide means arteries don’t relax as well. They become stiffer and less compliant.
- Inflammation Increases: The endothelium becomes “sticky,” allowing inflammatory cells and cholesterol to start building up in the artery wall (the beginning of atherosclerosis, or hardening of the arteries).
- ACE Activity May Increase: Some research suggests dysfunctional endothelial cells might produce more Angiotensin-Converting Enzyme (ACE), further ramping up the RAAS system and leading to more ANG II – causing even more stiffness and pressure [Source: Cardiovascular Research – Endothelium and ACE].
This stiffening is a huge deal.
Stiff arteries resist blood flow more (higher resistance). Your heart has to pump harder to push blood through. Pressure goes up.
Remember those baroreceptors (stretch sensors)? When arteries are chronically stiff, they don’t stretch normally. This can confuse the signaling to the brain.
Over time, the brain might interpret this altered signaling from stiff vessels as “normal,” gradually resetting the blood pressure “set point” higher.
Now, chronically elevated pressure is the norm for the body. This is a key part of the pathophysiology of hypertension.
This puts extra strain on the heart (leading to enlargement or heart failure over time) and damages delicate blood vessels in the kidneys and brain, increasing the risk of kidney failure and stroke.
It’s a cascade: Endothelial dysfunction → Arterial Stiffening → Increased Resistance → RAAS Activation → Higher Pressure → Baroreceptor Reset → More Endothelial Damage → Even Stiffer Arteries… and round and round it goes.
This process often starts silently, long before someone meets the criteria for hypertension stage 1 or hypertension stage 2.
The high blood pressure reading is a symptom appearing along this pathway. The root issue often begins with the health of the endothelium and the resulting arterial stiffness.
This is why focusing solely on the pressure number might be missing the earliest opportunity to intervene.
So, if arterial stiffness is such a crucial, early factor, how can we measure it? Traditionally, this wasn’t easy outside of specialized labs.
But technology is changing the game.
What are 5 signs of hypertension?
Again, most people have NO signs. Relying on symptoms is risky. However, very high or rapidly rising blood pressure (hypertensive crisis) might cause: severe hypertension headache, shortness of breath, nosebleeds, severe anxiety, confusion, vision changes, or chest pain. These require immediate medical attention. But for typical hypertension, there are usually no warning signs.
How does hypertension affect your life?
Untreated hypertension significantly increases your risk of heart attack, stroke, heart failure, kidney disease, vision loss, vascular dementia, and sexual dysfunction. It forces your heart to work harder and damages blood vessels over time. Managing it is crucial for longevity and quality of life.
When should you worry about high blood pressure?
You should take any high blood pressure reading seriously and discuss it with your doctor. Consistent readings above 130/80 mmHg warrant attention. Readings above 180/120 mmHg constitute a hypertensive crisis needing immediate medical care. Don’t wait for symptoms.
Measuring What Matters: Is Pulse Wave Velocity (PWV) the Missing Link?
For decades, the trusty blood pressure cuff (sphygmomanometer) has been the standard. It’s accessible, relatively easy to use, and gives us those two important numbers: systolic and diastolic pressure.
But it gives us a snapshot of the force at one moment in time. It doesn’t directly tell us about the condition of the artery wall itself – its stiffness or elasticity.
Imagine trying to judge the health of a garden hose just by measuring the water pressure at the nozzle. It tells you something, but not whether the hose itself is becoming brittle and likely to crack.
This is where Pulse Wave Velocity (PWV) comes in.
Think about dropping a pebble in a pond. Ripples spread outwards. Similarly, each time your heart beats, it sends a pressure wave (pulse) traveling down your arteries.
PWV measures the speed at which this pressure wave travels through your arterial tree, usually measured between the carotid artery in your neck and the femoral artery in your leg.
Here’s the key insight: The stiffer the artery, the faster the pulse wave travels.
Think of tapping a steel pipe versus a flexible rubber tube. The vibration travels much faster through the rigid steel.
PWV provides a direct, non-invasive measure of arterial stiffness. And a growing body of scientific evidence highlights its importance:
- Predictive Power: Studies consistently show that higher PWV (indicating stiffer arteries) is a strong, independent predictor of future cardiovascular events like heart attack and stroke, sometimes even better than traditional blood pressure readings alone [Source: European Heart Journal – PWV as a cardiovascular risk marker].
- Early Warning: Arterial stiffness often starts increasing before blood pressure becomes clinically high (hypertension stage 1). Measuring PWV could potentially offer an earlier warning sign of trouble brewing.
- Reflects Vascular Age: PWV is considered one of the best biomarkers for “vascular age”—meaning how old your arteries are functionally, regardless of your chronological age. Stiffer arteries mean an older vascular age, even in young adults (what causes high blood pressure in young adults is often linked to early vascular stiffening).
Until recently, measuring PWV required expensive equipment (costing thousands of dollars) and trained operators, confining it mostly to research labs and specialized clinics.
This is why it hasn’t been part of routine checkups. Why focus on stiffness if you couldn’t easily measure it? It was easier to stick with the readily available blood pressure measurement.
But technology marches on.
As the original article mentioned, devices are now emerging that bring PWV measurement into the home. Certain smart scales, for example, can estimate PWV using sensors you stand on during your regular weigh-in.
Disclaimer
Like the original author, I have no affiliation with any specific brand. The mention of technology like the Withings Body Cardio scale is purely illustrative of the trend towards accessible PWV monitoring. Always do your own research and consult healthcare professionals regarding health devices and data interpretation.
Having access to this kind of data – tracking your PWV trends over time alongside your blood pressure – could be incredibly empowering.
It shifts the focus from just managing a number (pressure) to understanding and influencing the underlying health of your arteries (stiffness).
If your PWV starts trending up, even if your blood pressure is still technically “normal,” it could be a powerful motivator to double down on healthy lifestyle habits before hypertension fully develops.
And if you already have hypertension, tracking PWV might help you see more quickly which lifestyle changes are effectively reducing arterial stiffness, potentially even before the changes fully reflect in your blood pressure readings (remember, resetting that baroreceptor set point takes time).
This brings us to the most important part: What can you actually do?
How to down blood pressure? / How do I lower my blood pressure?
Lifestyle changes are key: adopting a heart-healthy diet (like DASH), reducing sodium, increasing physical activity, losing excess weight, managing stress, limiting alcohol, and quitting smoking. Medication is often necessary as well, prescribed by a doctor.
Can dehydration cause high blood pressure?
Yes, sometimes. Dehydration can cause blood volume to decrease, signaling the body (via RAAS) to constrict blood vessels to maintain pressure. It can also make blood thicker. Staying well-hydrated is important for overall cardiovascular health.
Taking the Wheel: Strategies for Healthy Arteries and Blood Pressure
Okay, we’ve journeyed through the complexities of hypertension, flow vs. pressure, RAAS, endothelial function, and arterial stiffness.

The core message emerging is that the health of your arteries is paramount. Stiff arteries often precede or accompany high blood pressure.
So, the most powerful approach involves strategies that promote flexible, healthy arteries and support overall cardiovascular wellness. This is the foundation of both prevention of hypertension and effective management.
The good news? You have significant control here. While medication plays a vital role in hypertension treatment for many, lifestyle interventions are the bedrock. They target the root causes we’ve discussed.
Let’s break down the most impactful strategies:
1. Move Your Body (The Non-Negotiable!)
The original article called exercise the “strongest anti-hypertensive drug,” and it’s hard to argue with that. Regular physical activity is phenomenal for your arteries.
- Boosts Nitric Oxide: Exercise stimulates your endothelium to produce more NO, promoting vasodilation (relaxation) and flexibility.
- Improves Endothelial Function: It helps heal and maintain a healthy endothelial lining.
- Lowers Inflammation: Regular movement combats chronic inflammation throughout the body.
- Helps Manage Weight & Stress: Both are major factors in blood pressure control.
- Strengthens the Heart: Makes your heart more efficient.
What kind of exercise? A mix is usually best:
- Aerobic Exercise: Activities that get your heart rate up for a sustained period (brisk walking, jogging, cycling, swimming, dancing). Aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity activity per week, as recommended by the American Heart Association [Source: AHA Recommendations for Physical Activity].
- Resistance Training: Working your muscles with weights, resistance bands, or bodyweight exercises at least twice a week helps improve metabolic health and body composition.
- HIIT (High-Intensity Interval Training): As mentioned in the original article, short bursts of intense effort followed by brief recovery can be very time-efficient and effective for improving cardiovascular fitness and potentially lowering blood pressure and stiffness [Source: British Journal of Sports Medicine – HIIT and blood pressure].
The key is consistency. Find activities you enjoy and make them a regular part of your life. Even short walks count!
2. Fuel Wisely: Your Diet Matters Immensely
What you eat directly impacts endothelial function, inflammation, RAAS activity, and ultimately, arterial stiffness and blood pressure.
Focus on a whole-foods-based approach:
- Load Up on Plants: Fruits, vegetables, legumes (beans, lentils), whole grains. They are packed with vitamins, minerals, fiber, and antioxidants that protect your endothelium.
- Prioritize Potassium: This mineral helps balance out the effects of sodium and relaxes blood vessel walls. Find it in bananas, sweet potatoes, spinach, beans, yogurt, and avocados.
- Get Enough Magnesium: Involved in hundreds of bodily processes, including blood pressure regulation and NO production. Good sources include leafy greens, nuts, seeds, and whole grains.
- Embrace Healthy Fats: Omega-3 fatty acids (from fatty fish like salmon, mackerel, sardines, plus walnuts, chia seeds, flaxseeds) are anti-inflammatory and support heart health. Olive oil is also excellent.
- Nitrate Power: Foods rich in natural nitrates can be converted to Nitric Oxide (NO) in the body. Think beetroot (as highlighted in the original article – juice or whole), spinach, arugula, celery, and lettuce. Studies support beetroot’s role in lowering blood pressure [Source: Journal of Nutrition – Beetroot Juice and BP].
- Fiber is Your Friend: Helps manage cholesterol, blood sugar, and weight. Aim for plenty from whole grains, fruits, vegetables, nuts, and seeds.
Equally important is what to limit or avoid – the high blood pressure foods to avoid:
- Excess Sodium: A major driver of fluid retention and high pressure for many. Cut back on processed foods, canned soups, fast food, salty snacks, and restaurant meals. Aim for less than 1,500 mg per day if you have high blood pressure, as advised by the AHA. Read labels!
- Added Sugars: Found in sugary drinks, sweets, and many processed foods. Excess sugar contributes to inflammation, weight gain, and endothelial dysfunction.
- Unhealthy Fats: Limit saturated fats (fatty meats, full-fat dairy) and avoid trans fats (often in processed baked goods and fried foods).
- Refined Grains: White bread, white rice, pastries – choose whole-grain options instead.
- Excessive Alcohol: Can raise blood pressure significantly. Limit intake according to health guidelines (e.g., up to one drink per day for women, up to two for men).
Think patterns like the DASH (Dietary Approaches to Stop Hypertension) diet or the Mediterranean diet, both rich in plants, lean proteins, and healthy fats, and proven effective for heart health.
3. Master Your Stress
We talked about how chronic stress keeps your sympathetic nervous system firing and can activate RAAS. Finding healthy ways to cope is crucial.
- Mindfulness & Meditation: Proven techniques to calm the nervous system and lower stress hormones [Source: JAMA Internal Medicine – Meditation and BP]. Even 5-10 minutes daily can help.
- Deep Breathing Exercises: Simple, yet powerful for activating the relaxation response.
- Yoga & Tai Chi: Combine movement, breathing, and mindfulness.
- Quality Sleep: Aim for 7-9 hours per night. Poor sleep is linked to higher blood pressure. Create a relaxing bedtime routine.
- Time in Nature: Spending time outdoors has restorative effects.
- Hobbies & Social Connection: Make time for activities you enjoy and connect with loved ones.

4. Maintain a Healthy Weight
Carrying excess weight, especially around the abdomen, puts extra strain on your heart and is strongly linked to high blood pressure, insulin resistance, and inflammation. Even modest weight loss (5-10% of body weight) can make a significant difference.
5. Ditch the Tobacco
Smoking damages the endothelium almost immediately, constricts blood vessels, raises blood pressure, and dramatically increases your risk of heart attack and stroke. Quitting is one of the single best things you can do for your cardiovascular health.
6. Consider Supportive Nutrients & Botanicals
While lifestyle forms the foundation, certain nutrients and natural compounds can play a supportive role in maintaining cardiovascular health and promoting healthy endothelial function.

This is where high-quality supplements might complement your efforts, always alongside diet and exercise, and ideally discussed with your healthcare provider.
- Omega-3 Fatty Acids: As mentioned, these essential fats (EPA and DHA) are critical for heart health, reducing inflammation, and supporting healthy blood vessel function. If your diet is low in fatty fish, a quality supplement could be beneficial.
Vitaleap Suggestion
To ensure you’re getting adequate omega-3s, especially if fatty fish isn’t a regular part of your diet, consider a high-quality supplement like…

Forever Arctic Sea
It provides a balanced blend of EPA and DHA from fish and calamari oils, designed to support cardiovascular wellness.
- L-Arginine & Nitric Oxide Support: L-arginine is an amino acid that serves as a precursor to Nitric Oxide (NO). Supporting NO production is key for vasodilation and endothelial health.
Vitaleap Suggestion

Forever Argi+
It combines L-Arginine with a blend of antioxidant-rich fruit extracts. This formulation is designed to support NO production, promoting healthy circulation and cardiovascular function – a great complement to an active lifestyle.
- Antioxidant Power: Combating oxidative stress is crucial for protecting the endothelium. Vitamins C and E, CoQ10, and various plant compounds (polyphenols) act as antioxidants.
Vitaleap Suggestion
Supporting your body’s natural antioxidant defenses is vital.
Forever Aloe Vera Gel
Pure Forever Aloe Vera Gel is known for its soothing properties and contains various nutrients. Incorporating it into your daily routine can be a refreshing way to support overall wellness, complementing a diet rich in colourful fruits and vegetables.
For broad-spectrum antioxidant support alongside essential vitamins and minerals,

Forever Daily
Provides a blend designed to fill nutritional gaps and support overall health, including contributing to the protection of cells from oxidative stress.
- Magnesium & Potassium: Ensuring adequate intake of these minerals is vital for blood pressure regulation. While diet should be the primary source, supplementation might be considered if intake is low (consult your doctor).
Important Note: Remember, supplements are supplemental. They support, but do not replace, a healthy lifestyle or necessary medical treatment for hypertension.
Always choose high-quality products and discuss supplement use with your doctor, especially if you have existing health conditions or are taking medications. Frame these suggestions as part of a holistic approach focused on nourishing the body.
These lifestyle strategies aren’t just about lowering a number; they’re about fostering fundamental health from the inside out, promoting flexible arteries, a calm nervous system, and optimal function.
They address the potential root causes behind why pressure might rise in the first place.
How to avoid high blood pressure?
Focus on the lifestyle factors above: maintain a healthy weight, eat a balanced diet low in sodium and processed foods, exercise regularly, manage stress, don’t smoke, and limit alcohol. Regular checkups are also key for early detection.
Home remedy for high blood pressure?
The most effective “home remedies” are consistent lifestyle changes: diet (like DASH), exercise, stress reduction, weight management.
Specific foods like beetroot, garlic, hibiscus tea, and omega-3 rich fish are often mentioned, but they work best as part of an overall healthy pattern, not as standalone cures. Always work with your doctor.
What are the top 10 symptoms of high blood pressure?
This is tricky because there often AREN’T symptoms. If forced to list potential signs (usually of very high pressure), they might include: severe headache, fatigue/confusion, vision problems, chest pain, difficulty breathing, irregular heartbeat, blood in urine, pounding in chest/neck/ears, dizziness, nosebleeds. But relying on these is dangerous – get checked regularly.
Addressing Specific Concerns About Hypertension
While the core principles apply broadly, let’s touch on a few specific situations and questions that often come up:
Hypertension in Younger Adults: It’s a concerning trend – what causes high blood pressure in young adults?
While genetics can play a role, lifestyle factors are increasingly implicated: diets high in processed foods and sugar-sweetened beverages, sedentary lifestyles (more screen time, less movement), rising obesity rates, and increased stress levels.
Early onset essential hypertension often involves early signs of endothelial dysfunction and arterial stiffening. Addressing lifestyle proactively is crucial.
Hypertension in Women: Factors unique to women can influence blood pressure, including hormonal changes (pregnancy, menopause), and use of birth control pills.
What causes high blood pressure in women can also be linked to conditions like PCOS (Polycystic Ovary Syndrome). Hypertension in pregnancy, including gestational hypertension and preeclampsia, requires careful monitoring and management due to risks for both mother and baby.
Understanding Blood Pressure Numbers:
- What is normal blood pressure by age? While pressure tends to rise with age, the ideal target remains below 120/80 mmHg for most adults.
Guidelines don’t typically set different “normal” ranges based purely on age anymore, although treatment thresholds might be adjusted based on overall risk. Check resources like the American Heart Association for current guidelines. - High Diastolic Blood Pressure vs. High Systolic Blood Pressure: Systolic (top number) reflects pressure during heartbeats; diastolic (bottom number) reflects pressure between beats.
Historically, systolic was seen as more important, but research shows both are significant risk factors. Elevated diastolic pressure, especially in younger individuals, might indicate less elastic arteries.
Stage 1 hypertension and stage 2 hypertension criteria consider both numbers.
When Things Get Serious:
- Malignant Hypertension: This is a rare but severe form involving extremely high blood pressure that develops rapidly and causes organ damage (e.g., to kidneys, eyes, brain). It’s a medical emergency.
- Hypertensive Crisis: Defined as BP readings exceeding 180/120 mmHg. Requires immediate medical evaluation, whether or not symptoms are present.
Medication Context: It’s crucial to reiterate that while this article explores underlying mechanisms and lifestyle, high blood pressure medication is often necessary and life-saving.
Finding the best medicine for high blood pressure is a personalized process done with your doctor, considering your health profile, other conditions, and potential side effects.
The goal is often to use lifestyle changes to potentially reduce the need for medication or lower the required dosage, under medical supervision. Never stop or change medication without consulting your doctor.
Reclaiming Your Power in the Hypertension Narrative
So, let’s circle back to our initial question: Are we being “red-herringed” into focusing only on the pressure number when it comes to hypertension?
Perhaps “red-herringed” is strong, but maybe “incompletely focused” is fair.
The traditional model of diagnosing and treating high blood pressure based primarily on cuff readings has saved countless lives, and medication is a vital tool.
However, by understanding the deeper physiology – the critical roles of blood flow, endothelial health, and arterial stiffness – we gain a more holistic perspective.
We see that hypertension is often not just a disease of high pressure, but a symptom of underlying vascular changes. Changes that frequently begin silently with endothelial dysfunction and stiffening arteries, driven largely by lifestyle choices and chronic inflammation.
The exciting part? This understanding empowers us.
Instead of feeling like passive recipients of a diagnosis and a prescription, we can become active participants in nurturing our vascular health.
By focusing on:
- Moving our bodies regularly
- Fueling ourselves with whole, nutrient-dense foods (low in sodium, sugar, unhealthy fats)
- Managing stress effectively
- Maintaining a healthy weight
- Avoiding tobacco
- Potentially monitoring arterial stiffness (PWV) alongside blood pressure (as technology allows)
- Supporting our efforts with high-quality, targeted nutrition (like the supportive FLP products mentioned)
…we are directly addressing the roots of the issue. We’re working to keep our endothelium healthy and our arteries flexible.
This isn’t about rejecting conventional medicine; it’s about integrating deeper knowledge for more proactive and personalized health management. It’s about shifting from just treating a symptom (high blood pressure) to cultivating fundamental cardiovascular wellness.
As Professor Jarisch noted nearly a century ago, our fascination with the easily measured (pressure) might have overshadowed the importance of the essential (flow and vessel health).
Now, with growing knowledge and new tools, we have the chance to broaden our focus.
Your cardiovascular health is a long game. By understanding the players – pressure, flow, stiffness, endothelium, RAAS – and taking consistent, positive action, you can significantly influence the outcome.
Take this knowledge, explore the strategies, talk with your healthcare provider, and step confidently onto the path of proactive heart health. You’ve got this.
What are your thoughts on this perspective? Do you track metrics beyond blood pressure? Share your experiences or questions in the comments below!